Medical Device CROs Market – The Next Growth Opportunity
Numerous scientific and technological breakthroughs in the medical device industry, over the past decade, have resulted in an accelerated pace of research and innovation within this domain. Further, the demand for advanced and minimally invasive medical devices has been augmented due to the increase in expenditure on healthcare. However, one of the primary challenges faced by this industry is the complex and time-consuming product development lifecycle of a new medical device. Specifically, the clinical stage is exceedingly resource intensive, involving high costs and greater risks. Furthermore, new advancements have facilitated the development and enforcement of more informed regulatory guidelines and instructions to ensure the safety of medical devices. Subtle differences in regulatory guidelines issues across various geographical regions need to be considered by medical device developers in order to receive approval in different markets. This has further resulted in longer trials, higher costs (due to rise in patient enrollments), and increased time-to-market. In order to overcome the abovementioned challenges, medical device developers are actively outsourcing their clinical research and associated operations to contract service providers, which are known to have the required capabilities and expertise.
Role of CROs in the Medical Device Industry
According to a SelectUSA.gov publication, the US has the largest medical device market of over USD 150 billion across the globe. In 2017, the US represented 40% of the global medical device market. Increasing healthcare expenditure, technological development, growth in aging population and rising incidence of chronic diseases have emerged as the key drivers for the growth of this market. Further, as per a report published by the World Bank, more than 50,000 types of medical devices are presently used in healthcare facilities worldwide.
Lately, medical devices companies have been facing the challenge of generating more clinical evidence for regulatory authorities, payers, physicians, and patients alike. Further, the establishment of stringent regulations, such as the new MEDDEV 2.7/1 Rev4 European regulation (published in 2017), has forced manufacturers to develop devices that include supporting equipment, delivery tools and software versions to prove their safety. As per the revised regulations, all new devices must be checked rigorously for quality, and the study data generated during the trial needs to be reported separately. This has compelled device manufacturers to run more and / or larger clinical trials. According to ClinicalTrials.gov, the number of medical device trials increased 94% from 2012 to 2017. In addition, manufacturers are increasingly conducting clinical trials in order to differentiate their products from competitors and enhance adoption rates amongst patient population.
However, majority of the device manufacturers lack the required internal resources and expertise to run a complete clinical trial and regulatory document submissions in-house. This is particularly true for smaller firms that have little experience and lack time, money and an established regulatory department. The past few years have witnessed medical device developers seeking the services of CROs for assistance with clinical operations management, investigator recruitment, clinical monitoring, data management, biostatistical analysis, quality assurance, regulatory approval, and other crucial operations.
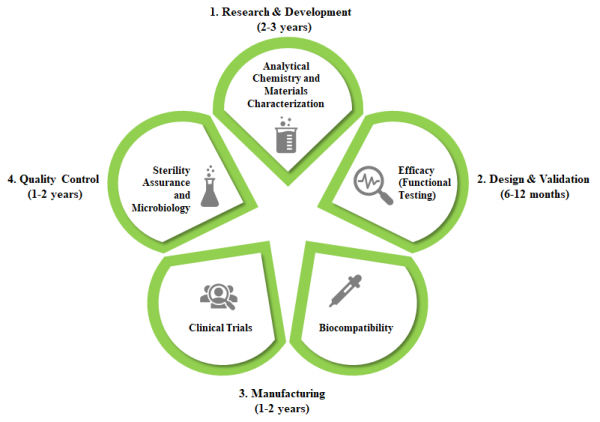
The growing demand for these devices calls for more and faster approvals. However, as discussed earlier, medical device development process is fairly complex and time-consuming (usually 10-12 years long); it usually progresses through the following stages:
- Research and Development: At this stage, the device undergoes certain screening and qualification tests, used to chemically characterize the medical device raw materials or components. It usually takes 2-3 years for a device to get through this stage.
- Functional Testing: This phase involves functionality testing, usually surgical studies that evaluate the performance of the device for intended use. It is generally a 6-12 months long process.
- Biocompatibility Testing: This step involves both in vitro and in vivo studies to ensure that the device is biologically safe for its intended use. It takes around 1-2 years for the device to qualify for the next stage of development.
- Clinical Trials: This stage includes scientific studies in human subjects, to evaluate a medical device for the treatment, prevention or diagnosis of a particular clinical condition. This phase is usually 1-2 years long.
- Sterility Assurance and Microbiology: This phase, which generally lasts 1-2 years, includes sterility validation, environmental monitoring, packaging validation and shelf-life testing. After the completion of this stage, the device undergoes various regulatory compliance checks before its launch.